Articles & Research
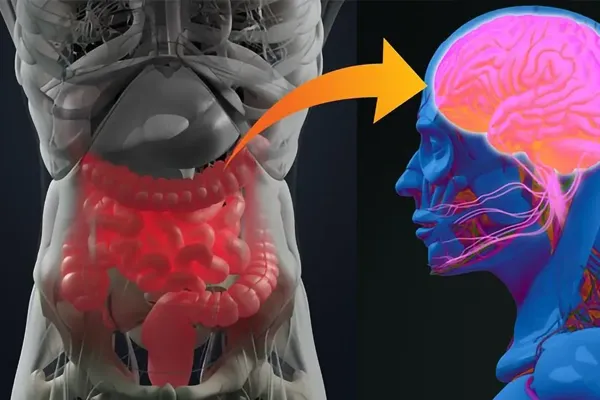
Gut Feeling: How the Gut–Brain Axis Affects Our Mood
The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health
Abstract
The gut-brain axis is a bidirectional communication network that links the enteric and central nervous systems. This network is not only anatomical, but it extends to include endocrine, humoral, metabolic, and immune routes of communication as well. The autonomic nervous system, hypothalamic-pituitary-adrenal (HPA) axis, and nerves within the gastrointestinal tract, all link the gut and the brain, allowing the brain to influence intestinal activities, including activity of functional immune effector cells; and the gut to influence mood, cognition, and mental health.
The gut-brain axis is a bidirectional communication network that links the enteric and central nervous systems. This network is not only anatomical, but it extends to include endocrine, humoral, metabolic, and immune routes of communication as well. The autonomic nervous system, hypothalamic-pituitary-adrenal (HPA) axis, and nerves within the gastrointestinal (GI) tract, all link the gut and the brain, allowing the brain to influence intestinal activities, including activity of functional immune effector cells; and the gut to influence mood, cognition, and mental health.
Clinical, epidemiological, and immunological evidence suggest that enteric microbiota extensively and profoundly influences the gut-brain relationship (ie, mental state, emotional regulation, neuromuscular function, and regulation of the HPA). Research continues to elucidate mechanisms of action to explain the effects of microbiota, both directly and indirectly, on emotional and cognitive centres of the brain1 and has demonstrated that fluctuations of the microbiota are linked to changes within these systems of communication.2
For example, several mood disorders, such as anxiety, depression, and autism spectrum disorders now have well-established links to functional GI disruptions, whereas GI disease (eg, irritable bowel syndrome, irritable bowel disease) often involve psychological comorbidities associated with alteration of the gut microbiome.3-9 In addition, research has demonstrated that the composition of gut bacteria appears to be influential in fetal and neonatal neurologic development.10 And, not surprising, diet has also been shown to influence the gut microbiome’s impact on cognitive function.11
Pathways of the Gut-Brain Axis
As early as 1998, oral administration of a single, unique bacterium (Campylobacter jejuni) to rats in subclinical doses was found to lead to anxiety-like behavior, without an accompanying immune response.12 Later research confirmed that introduction C jejuni caused anxiety-like behavior in mice, with concomitant activation of neuronal regions in the brain that were dependent on information received from the gut via the vagus nerve.13
The seminal first studies establishing mechanisms of the gut-brain axis made use of animals raised in a sterile environment. Sudo et al14 sought to answer the question of whether postnatal microbial colonization could affect the development of brain plasticity and subsequent physiological response. To test the idea that gut microbes might affect the development of neural systems that govern the endocrine response to stress, they studied the HPA axis reaction to stress by comparing germ-free (GF), specific pathogen free (SPF) and gnotobiotic mice. They found that colonizing microbes altered the HPA response to restraint stress, indicating that the interaction of gut bacteria with the brain is also bidirectional, just like the brain-gut axis. This was the first report to show commensal microbes affecting the neural network responsible for controlling stress responsiveness. In this study, the HPA response of the GF mice was more sensitive to restraint stress than that of the SPF mice, whereas both groups of mice failed to show any difference in the sensitivity to ether stress. In addition, GF mice exhibited reduced brain-derived neurotrophic factor (BDNF) expression levels in the cortex and hippocampus relative to SPF mice. The authors concluded:
Because the HPA response to restraint stress is affected by the limbic system, including the prefrontal cortex, hippocampus and amygdala, and requires assembly and processing of signals from multiple sensory modalities before initiation of a stress response, whereas ether stress does not…, these results indicate that cognitive processing in the limbic system may be involved in an exaggerated HPA response by GF mice.
Their study showed that commensal microbiota are an environmental determinant that regulates the development of the HPA stress response, and that the series of events in the GI tract following postnatal microbial colonization can have a long-lasting influence on the neural processing of sensory information regarding the endocrine stress axis.
In the decade since this groundbreaking research, these findings have been corroborated and expanded. For example, administration of oral antimicrobials to SPF mice was shown to transiently alter the composition of the microbiota and increase exploratory behavior and hippocampal expression of brain-derived neurotropic factor (BDNF), a key protein involved in neuronal plasticity and cognition.15 These changes were independent of inflammatory activity, changes in levels of GI neurotransmitters, and vagal or sympathetic integrity, leading the authors to conclude that intestinal microbiota influences brain chemistry and behavior independently. Other related research has shown that administration of Lactobacillus rhamnosus beneficially altered brain expression levels of BDNF and of genes involved in serotonin signaling and metabolism in zebrafish.16
A great deal of research, well beyond the scope of this review, has further elucidated 4 major pathways of the gut-brain axis: neurologic, endocrine, humoral/metabolic, and immune.
Neurologic Pathway
The neurologic pathway includes the vagus nerve, the enteric nervous system, and the activity of neurotransmitters within the GI tract. Neurologic modulation of afferent sensory nerves directly produces molecules that can act as local neurotransmitters, such as GABA, serotonin, melatonin, histamine, and acetylcholine; this pathway also generates biologically active forms of catecholamines in the lumen of the gut.2 The autonomic nervous system also influences immune system activation in the gut, for example by directly modulating macrophage and mast cell responses to luminal bacteria. In addition, the gut microbiome appears to be essential for normal gut intrinsic primary afferent neuron excitability.17
Endocrine Pathway
Gut microbiota alters nutrient availability and thus influences the release of biologically active peptides from enteroendocrine cells, which in turn can affect the gut-brain axis. For example, the neuropeptide galanin is thought to be involved in many critical neurobiological functions including nociception, sleep/wake cycle regulation, feeding, mood, blood pressure regulation, parental behavior, and neurotrophic functions. Galanin stimulates the activity of the central branch of the HPA axis (influencing release of corticotropin-releasing factor and adrenocorticotropic hormone), and thus enhances glucocorticoid secretion from the adrenal cortex.18 In addition, it is able to directly stimulate cortisol secretion from the adrenal cortex, as well as norepinephrine release from the adrenal medulla, demonstrating its involvement in the HPA axis response to stress.19
Humoral/Metabolic Pathway
Bacterial metabolites (most importantly short-chain fatty acids [SCFAs], produced by the bacterial fermentation of dietary carbohydrates) are decisive humoral influencers. Best known to affect the nutrition of enterocytes, they also exert significant hormone-like activity, have immunomodulatory properties, and interact with nerve cells by stimulating the sympathetic branch of the autonomic nervous system. Furthermore, microbiota-derived SCFAs are able to cross the blood-brain barrier and have been shown to regulate microglia homoeostasis, which is required for proper brain development and brain tissue homoeostasis, and is involved in behavior modulation.20 Of important note, disruptions to SCFA metabolism have been implicated in the development of autism through the disruption of microglial communication and function.21-24 SCFAs also regulate the release of gut peptides from enteroendocrine cells and have been shown to regulate the synthesis of gut-derived serotonin from enterochromaffin cells, both of which in turn affect gut–brain hormonal communication.25 The gut provides approximately 95% of total body serotonin, most of which exists in plasma. Although serotonin has intrinsic roles in the intestines and peripheral metabolism, it is capable of locally activating afferent nerve endings that are connected directly to the central nerve system. 22 Although most physicians are familiar with the fluoxetine’s mechanism of blocking the transport of gut serotonin into plasma, many are unaware that elevated plasma serotonin has been observed in children with autism.26,27 An inverse correlation between high plasma serotonin and low serotonergic neurotransmission has been demonstrated in young male adults with autism spectrum disorder. 22
Another decisive bacterial metabolite is lipopolysaccharide (LPS), which is principally derived from the cell walls of Gram-negative enterobacteria. LPS gains entry to the systemic circulation via intestinal epithelial tight junction permeability defects, colloquially known as leaky gut syndrome. The human body produces antibodies against LPS, and their levels are known to be higher in patients with major depression than in controls.28
Immune Pathway
Inflammation metabolism within the GI tract is influenced by the gut microbiome, principally via the immune systems release of cytokines (such as interleukin [IL]-10 and IL-4) and other cellular communication mediators, such as interferon-gamma, during times of dysbiosis. In irritable bowel syndrome (IBS), as an example, abnormal microbiota populations activate mucosal innate immune responses, which increases gut epithelial permeability, activates gut pain sensory pathways, and dysregulates the enteric nervous system2,29,30; both brain-gut and gut-brain dysfunctions occur, the former being dominant.31 Disruptions in the gut-brain axis affect intestinal motility and secretion, contribute to visceral hypersensitivity and lead to cellular alterations of the entero-endocrine and immune systems.2
Epithelial Barrier Structure and Function
Stress is now well demonstrated to alter intestinal epithelial permeability, permitting bacterial antigens and LPS to enter circulation and become humoral influencers, with wide-ranging effects.32-36 In vivo experiments have shown that acute stress acts on the GI tract by inducing changes in colonocyte differentiation and decreased expression of mRNA encoding tight junction proteins.37
Intestinal permeability defects have been associated with a number of gut-related disorders, such as irritable bowel syndrome (IBD), necrotizing enterocolitis, and the low-level inflammation commonly seen in metabolic syndrome, obesity, and diabetes.38 So-called leaky gut is seen in some subtypes of IBS, such as that which commonly follows an infectious etiology,39 as well as in some forms of allergy.40 It should come as no surprise, then, that supplementation with probiotics could influence intestinal tight junction integrity, and thus support resolution of conditions caused or exacerbated by gut barrier dysfunction. Few clinical trials of probiotics have directly investigated epithelial barrier function in humans, but evidence is emerging in support of using lactobacilli for this purpose.41,42
For example, a multistrain combination of lactobacilli, lactococci, and bifidobacteria (Ecologic BARRIER, Winclove, Amsterdam, Netherlands) has demonstrated in vitro strengthening of the epithelial barrier after a pathogenic bacterial and inflammatory stressors, inhibition of mast-cell activation, stimulation of anti-inflammatory cytokine IL-10, and decreased LPS load.43 This preclinical work formed the basis for later clinical evidence of efficacy in preventing depression, discussed in the next section.
Inflammation, Depression, and the Microbiome
Studies from animal models conducted by independent research groups have corroborated findings of gut dysbiosis and its relation to monoamine disruptions seen in clinical depression, connecting gut microbiota with mood.44-48 In addition, intestinal permeability defects are thought to underlie the chronic low-grade inflammation observed in stress-related psychiatric disorders.49 Those with symptoms of depression frequently exhibit increased expression of proinflammatory cytokines, such as IL-1β, IL-6, tumor necrosis factor-α, as well as interferon gamma, and C-reactive protein.50-51,52 Gut microbiota influence transcription of these same cytokines, with dysbiosis triggering the so-called inflammasome pathway, whereas beneficial metabolites (SCFAs in particular) reduce production of proinflammatory cytokines, such as NF-κB.53
Gut microbiota are well known to support tight junction integrity between enterocytes. It should therefore come as no surprise that dysbiosis and associated increases in intestinal permeability are now recognized features of rheumatoid arthritis, Alzheimer’s disease, asthma, autism spectrum disorders, and other systemic conditions both inflammatory and otherwise. In recent years, there has been a tremendous amount research validating the mechanisms and role of the microbiome and probiotics in managing inflammatory conditions, particularly IBD.54-59
Depression is increasingly recognized as having an inflammatory component; indeed, anti-inflammatory drugs, such as COX-2 inhibitors, have previously demonstrated efficacy in major depression.60 Research has demonstrated that an inflammatory phenotype alters neurotransmitter metabolism by reducing the availability of neurotransmitter precursors and activating the HPA axis, all of which contribute to the pathogenesis of clinical depression.61,62 Although introduced as early as 1910,63 it has taken over a century for converging aspects of research to establish the gut-brain axis as a critical pathway to the effective prevention and treatment of clinical depression.64,65 Preclinical research laid the groundwork to investigate the use of probiotics for the treatment of mood disorders in humans.
Clinical Trials in Humans
A new class of probiotics, known as psychobiotics or psychomicrobiotics, has emerged in the last decade and is being fervently embraced by many health care practitioners as a nontoxic intervention for various psychiatric conditions.66,67 Several clinical trials have now documented effects, or lack thereof, of certain probiotics for depression and anxiety.
2002: In a pre- and postintervention assessment of adults suffering from stress or exhaustion (N = 34), a combination of L acidophilus, B bifidum and B longum improved subjects’ general condition by 40.7% after 6 months.68
2004: In a prospective, randomized, controlled, parallel study of healthy students (N = 136), researchers found no significant effects of L casei supplementation on anxiety levels, although beneficial alterations of lymphocyte and CD56 cell counts were observed.69
2007: In randomized, double-blind trial (N = 124), consumption of probiotic-containing yogurt had no effect on profile of mood states results, although there was improved self-reported mood of those whose mood was initially poor.70
2009: In a double-blind, randomized, placebo-controlled pilot study (N = 35, chronic fatigue syndrome patients), 2 months’ Anxiety Inventory supplementation with L casei significantly improved Beck scores. There was no effect on Beck depression inventory scores.71
2011: In subjects with reduced urinary free cortisol, consumption of the probiotics reduced anxiety and depression scores.72
2011: In a double-blind, randomized, controlled, parallel study (N = 55), consumption of L helveticus and B longum reduced somatization, depression, and anger-hostility as well as hospital anxiety and depression scale global scores; self-blame score on coping checklist and increased focus on problem solving, but there was no effect on perceived stress.73
2014: In a randomized, double-blind study (N = 36), L helveticus supplementation for 12 weeks had no significant effects on the perceived stress scale or geriatric depression scale; improvements were noted, however, on the digit span test, story recall test, verbal learning test, rapid visual information-processing, and stroop tasks scores.74
2015: In self-report questionnaires on fermented food consumption, neurosis, and social anxiety in young adults (N = 710), consumption of fermented foods containing probiotic bacteria was inversely associated with social anxiety and neurosis. Those at higher genetic risk for social anxiety disorder (indexed by higher tendency to neurosis) exhibited fewer social anxiety symptoms when they consumed more fermented foods.75
2015: The effects of a multistrain probiotic formula (Ecologic BARRIER, Winclove, Amsterdam) was tested in a randomized, triple-blind, placebo-controlled trial (N = 40 nonsmoking healthy young adults, mean age 20 y).76 The formula contained specific strains of B bifidum, B lactis, L acidophilus, L brevis, L casei, L salivarius, and L lactis at a dose of 5 billion colony-forming units (CFUs) per day. Consumption of this multispecies probiotic significantly reduced overall cognitive reactivity to depression, in particular aggressive and ruminative thoughts, as assessed by the Leiden index of depression sensitivity. This study is noteworthy because many patients, especially in young people with no prior history of depression, would prefer nonpharmaceutical interventions as a first-line treatment.77
2016: In randomized, double-blind study (N = 40), administration of a combination of L acidophilus, L casei, and Bifidobacterium bifidum for 8 weeks improved scores on the beck depression inventory.78
In a 2017 systematic review by Wallace and Milev of 10 clinical trials, most of the studies found positive results on measures of depressive symptoms.61 Because clinical trials on probiotics for depression and anxiety have been heterogeneous in terms of dosing, probiotic strain selection, and length of treatment, further randomized controlled clinical trials are warranted to validate the efficacy of this promising intervention.
Biography
Jeremy Appleton, ND, is a writer and speaker on topics in natural medicine and dietary supplements. An alumnus and former faculty member of the National University of Naturopathic Medicine, Dr Appleton is a licensed naturopathic physician, author, educator, and vice president of science and education for SFI USA, which manufactures dietary supplements under the Klaire Labs brand.

